Insulin is the cornerstone of treatment for most diabetic cats. On this page, you’ll find everything you need to know to get started—from choosing the right type of insulin and giving injections, to monitoring blood sugar at home and avoiding dangerous lows. We’ll walk you through safe dosing, proper technique, feeding tips, emergency preparedness, and building a routine your cat can live with. Whether you’re just starting out or looking to fine-tune your cat’s care, this guide is here to help.
Understanding Insulin Treatment
Once your cat is diagnosed with diabetes, insulin therapy may be necessary to manage high blood sugar levels and prevent complications. While some cats can achieve remission with diet alone, many require daily insulin injections to bring their glucose levels into a safe range. Modern veterinary guidelines, such as those from the American Animal Hospital Association (AAHA), provide a standardized approach to feline diabetes care. These guidelines encourage collaboration between pet owners and vets, and you may want to share them with your vet to ensure they’re current with best practices.
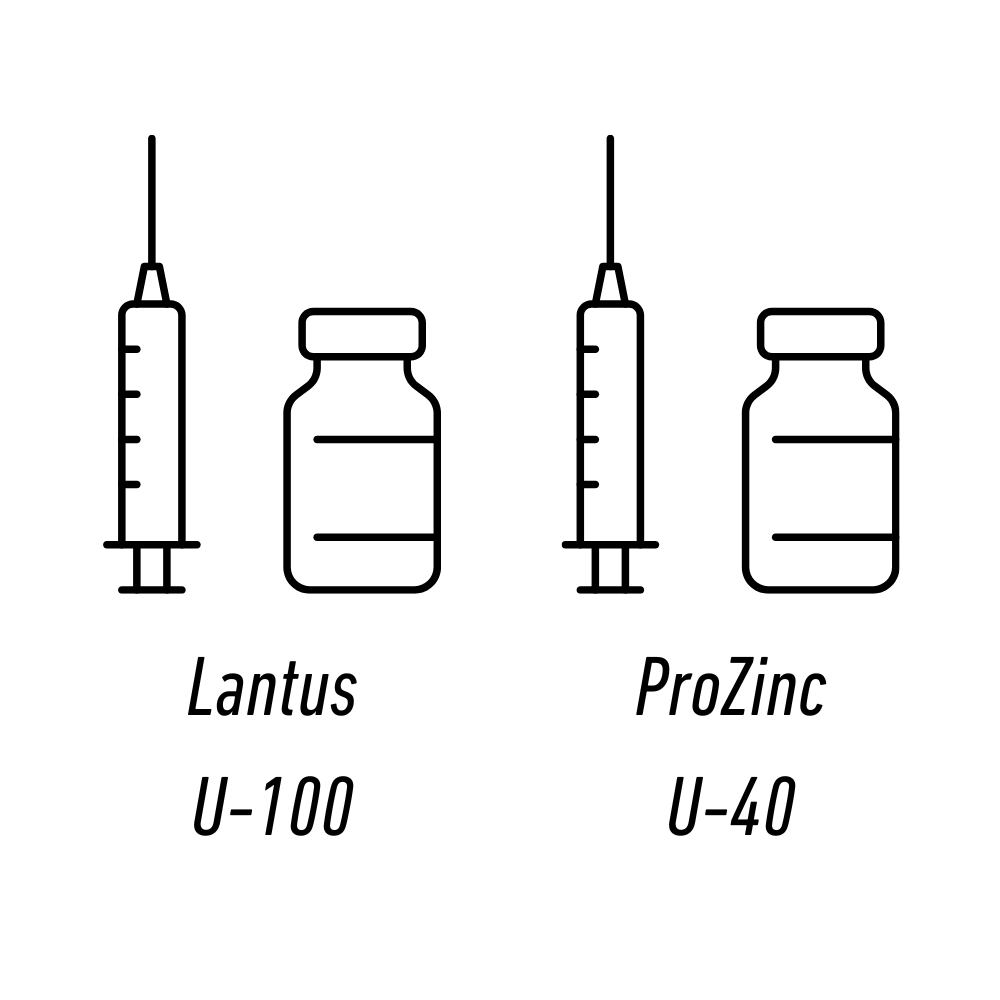
Choosing the Right Insulin
Not all insulins are created equal for cats. The most recommended options are glargine (Lantus) and detemir (Levemir) due to their gentle, predictable action. Protamine zinc insulin (PZI) is also used, though less commonly. Avoid Humulin N and Vetsulin, as they tend to cause erratic results in cats. It’s essential to match your insulin with the correct syringe type—U-40 or U-100—as mismatched dosing can lead to dangerous mistakes. If you must use a mismatched syringe, use a reliable conversion chart to ensure safe dosing.
Starting Insulin: Go Slow
When beginning insulin therapy, a cautious approach is safest. Most cats should start on 1 unit or less every 12 hours, with adjustments made slowly—no more than 0.5 to 1 unit at a time and typically in 0.25 unit increments. The full effect of a dose may take several days to observe, and rushing changes can increase the risk of hypoglycemia (low blood sugar), a potentially fatal condition. Regular checkups and re-evaluation after the first week are key, even if you’re home-testing.
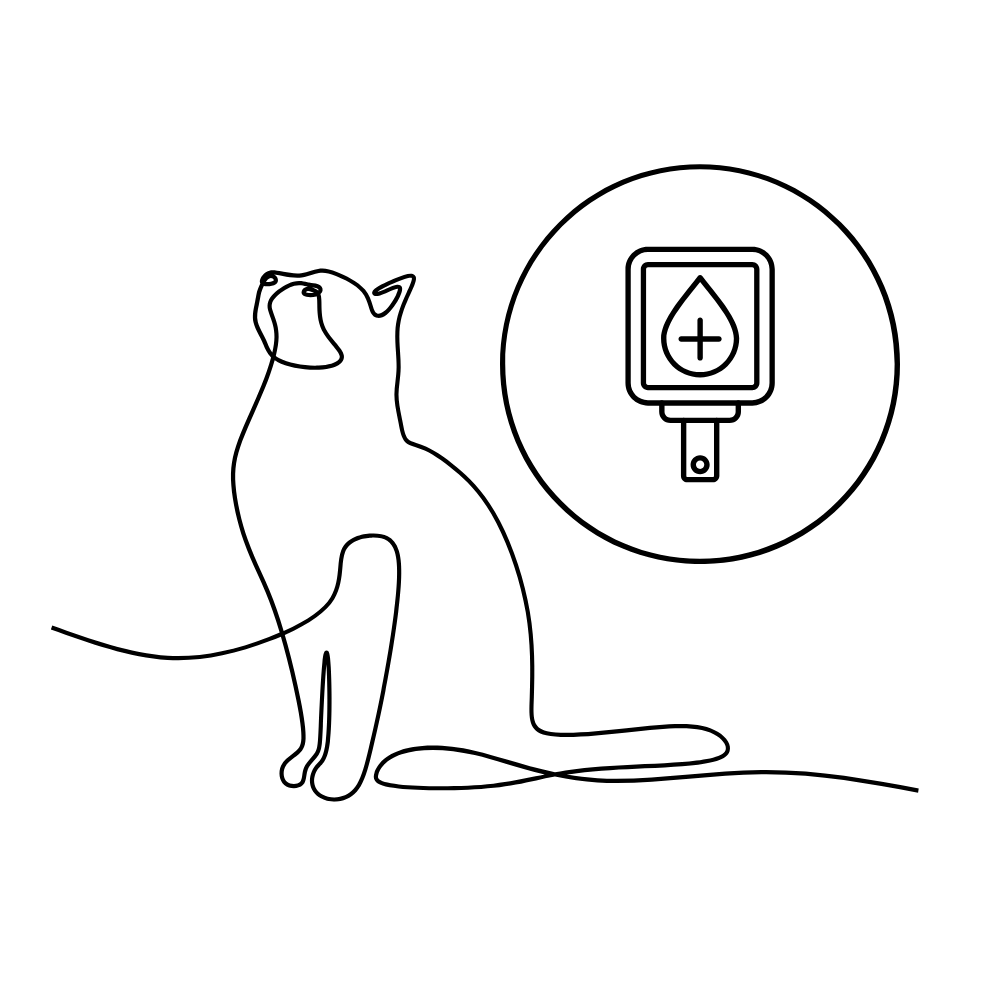
Home Testing and Monitoring
Home blood glucose testing is strongly recommended. A simple human glucometer can provide real-time data, allowing you to see how your cat responds to insulin. This is more accurate than urine testing and allows you to identify your cat’s nadir—the lowest blood glucose point in the cycle. Monitoring pre-injection levels alone isn’t enough, as high readings can mask dangerously low nadirs. Consistent home testing helps you and your vet make safe dosing decisions and avoid rebound effects or overdosing.
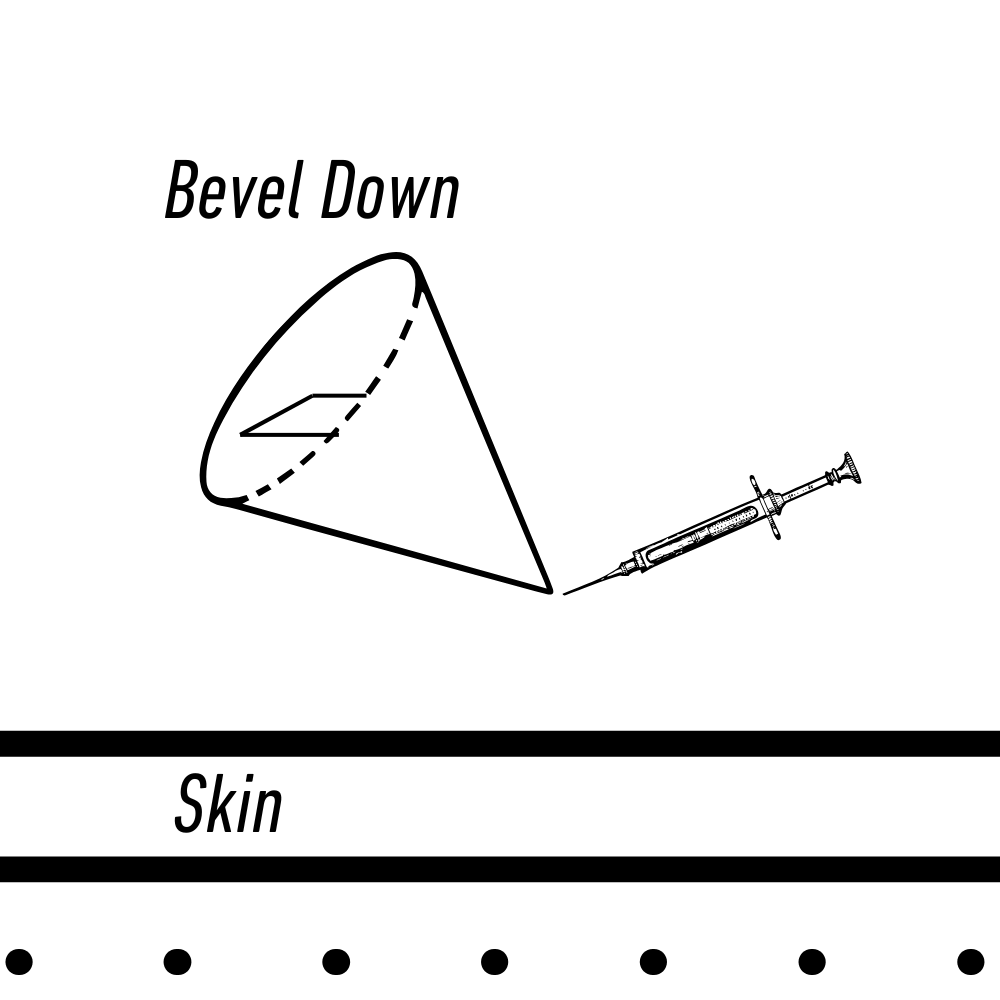
Injection Techniques and Tips
Giving insulin injections may seem intimidating at first, but with routine and technique, it becomes second nature. Always inject subcutaneously (under the skin), not into muscle. Most people tent the skin between the shoulders or use the flanks or abdomen—areas with better absorption than the scruff. Rotate injection sites to avoid scar tissue buildup. Use ultra-fine needles and consider warming the insulin slightly in your fingers to reduce discomfort.
Developing a calm, predictable routine—feeding, petting, and then injecting—can help your cat become more tolerant. Some caregivers disguise the syringe or turn the injection into a game. Each cat is different; learning what works for yours is part of the journey.
Feeding and Insulin Timing
Diet plays a major role in diabetes management. Cats should be fed low-carbohydrate, high-protein wet food, like Fancy Feast Classics. Dry food, including prescription varieties, contains too many carbs and can interfere with glucose control. Always feed around the time of injection—ideally before or during—to ensure the body has glucose available when the insulin kicks in. If your cat refuses food, consider skipping insulin and contact your vet if fasting continues for 24 hours.
Emergency Preparedness: Hypoglycemia
Every caregiver should be prepared for hypoglycemia. Symptoms include weakness, disorientation, wobbling, or seizures. If you suspect a low blood sugar episode, immediately rub a sugar source like Karo syrup or honey on your cat’s gums—never squirt it into the mouth. Even if you’re on the way to the vet, repeat sugar application every few minutes until your cat stabilizes. Short-term high blood sugar is not dangerous, but hypoglycemia can kill quickly. Keep sugar on hand at all times and consider printing an emergency guide to keep in your home.
Vet Care and Adustments
Even with home monitoring, regular vet checkups are essential. Tests like fructosamine or A1c give a longer-term picture of control and should be done every 3–6 months depending on your cat’s regulation status. Diabetes can affect other organs, so annual full blood panels are crucial. As your cat’s diet, exercise, or health status changes, insulin needs may shift, so all adjustments should be gradual and guided by data.
Support, Encouragement, and Community
Managing feline diabetes can be challenging, especially at first. You’re not alone—thousands of caregivers are navigating this with their cats every day. The Feline Diabetes Management Board (FDMB) is a great place for support, questions, and encouragement. Build a team: your vet, backup caregivers, and an online support group can make all the difference. Many people find the first few weeks the hardest, but with time and consistency, both you and your cat will adjust. Don’t be afraid to ask questions, celebrate progress, and reach out for help.